Section A: Osteoporosis / Osteopenia

Q&A on the topic with the following questions in the following order:
- How is osteoporosis classified?
- How is osteoporosis diagnosed?
- What is osteoporosis and whats the difference to osteopenia?
- What is bone quality?
- What are common symptoms in people with osteoporosis?
- What do I need to be aware of when dealing with a patient with severe osteoporosis?
- What is really increasing fracture risk in older people?
- When and why should you get your BMD checked?
- Why do we develop osteoporosis?
- Can we prevent it? does lifestyle matter? or is it simply genetics?
- What about running? is that not enough for lower limb BMD?
- What can we do to reduce fracture risk?
- Does nutrition play a role?
- Is osteoporosis reversible?
- ”I was diagnosed with osteoporosis, can I continue running?"
- What's the "best'' intervention for osteoporosis/-penia (resistance training, balance, walking, running, combined?)
- Why exercise for osteoporosis?
- Can we alter falling mechanics to reduce fracture risk?
- What are the dangers of sustaining an osteoporotic fracture?
- Are there movements that I should not do with osteoporosis?
- Can we give every person with osteoporosis the same exercise protocol?
- What does an appropriate exercise selection for osteoporotic patients look like?
- What about training with / after vertebral fractures?
- Do higher training loads lead to greater bone adaptations?
Defintion:
In 1998 the WHO defined osteoporosis as "a disease characterized by low bone mass and microarchitectural deterioration of bone tissue, leading to enhanced bone fragility and a consequent increase in fracture risk".
- How is osteoporosis classified?
Primary Osteoporosis (95% of cases) (also called involutional osteoporosis)
Type 1 (postmenopausal):
- Affects women aged 50–70
- Cause: Hormonal change > Estrogen deficiency > increased bone resorption
- Mainly affects: Spongiosa
- Common fractures: Vertebrae, wrist, femoral head
Type 2 (senile):
- Affects women & men over 70 (ratio 2:1)
- Causes: lack of activity + protein, vitamin D, calcium deficiency
- Mainly affects: Cortical bone of long bones
- Common fractures: Hip (femoral neck), upper arm (humerus)
Secondary Osteoporosis (5% of cases)
- Affects men and women equally
Causes: Hormonal disorders, medications (e.g. corticosteroids, antiepileptics), alcohol, smoking, lactose intolerance, tumors, long-term immobility
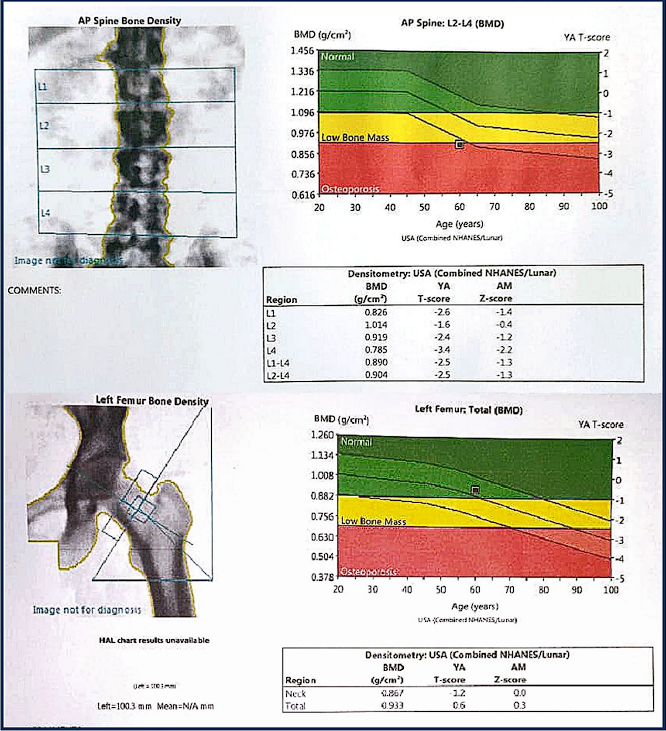
- How is osteoporosis diagnosed?
Osteoporosis is diagnosed with DEXA (Dual-Energy X-ray Absorptiometry). DEXA is a non-invasive imaging technique that measures the amount of bone mineral mass with CSA (cross sectioanl area) in g/cm2, using dual X-ray beams. By subtracting soft tissue, it provides a precise assessment of bone density, converting the result into a T-score. DEXA is quick, emits low radiation, and has a precision error of 1–2.5%. Measurements are taken at the femur neck, the spine (L1-L4) and sometimes the wrist. If multiple sites are measured, the lowest score accounts for the diagnosis.
- What is osteoporosis and whats the difference to osteopenia?
Osteoposrosis is a progressive disease affecting skeletal system that causes reduced bone mass and microstructural degradation of bone architecture. This changes increase bone fragility and fracture chance.
a) Bone mass (amount of bone present) and b) bone microarchitecture (material properties of the bone) are the two components that build our bones resilience.
Osteoporosis is defined as having a bone mineral density of at least 2,5 standard deviations below the average peak bone mass. This measure is defined as the T-score. And a T-score below -2,5 classifies someone as having osteoporosis, while a T-score of -1 to -2,5 gets you the label of osteopenia (=precursor of osteoporosis).
• ≥− 1.0: normal
• <− 1.0 to>− 2.5: osteopenia
• ≤− 2.5: osteoporosis
Clinically the diagnosis can be made in "people aged 50 years and older if they have sustained a low-trauma hip, vertebral, humerus or pelvic fracture" (Morin et al., 2023).
Since osteoporosis is solely determined by BMD, other bone properties are not considered when assessing bone quality.
- What is bone quality? is BMD the best assessment for quality?
Bone quality has been defined as "totality of features and characteristics that influence a bone’s ability to resist fracture" (Bouxsein, 2003).
Bone quality somewhat includes every bone characteristic (such as bone microarchitecture, turnover, bone mineral content and geometry) apart from BMD. Training interventions, although most often ranked by their effectiveness regarding BMD increases, are also believed to target aspects of bone quality (structural adaptations).
Therefore: Bone strength = Bone Density + Bone Quality
- What are common symptoms in people with osteoporosis?
Osteoporosis is an asymptomatic condition (also called a silent disease). It is oftentimes only recognised after sustaining a fracture by falling / getting hit with an amount of force that normally should not have led to a fracture (e.g. fall from standing height). Therefore, osteoporosis is a pain-free condition, until you suffer a fracture. It can be seen as a risk factor for fracture just as high blood pressure is for a stroke. Which means that it is impossible to know if you got it, so getting your BMD assessed is important when you get older (when exactly you should do so is explained elsewhere).
Other clinical signs seen in osteoporotic patients, apart from fractures, is height loss (especially in oder individuals). This stems form vertebral fractures that can occur spontaneously (without adequate trauma during ADLs), leading to vertebral compression. This becomes apparent when either height is measures or when the occiput-to-wall distance increases (due to increased thoracic kyphosis).
Sustaining a vertebral fracture increases risk for subsequent vertebral fractures as well as fractures in other body parts.
Fractures in other body parts (especially at the hip) are associated with higher mortality rates in the following year. Making fracture prevention and risk assessment a key priority for susceptible individuals.
This leaves us two therapeutic options:
- Reduce risk of falls (e.g. via balance exercise).
- Increase bone mass / density (e.g. via exercise or medication)
- What do I need to be aware of when dealing with a patient with severe osteoporosis?
It is important to include some sort of a future risk assessment to know who you are dealing with.
As osteoporosis is mainly a risk factor for fractures, we need to assess a persons risk of fracture to derive consequences. The FRAX (fracture risk assessment tool) has been developed to do just that. It uses personal data to calculate a fracture risk in %, which can then be used to classify persons for different treatment options. The 10 year fracture risk as measured via FRAX can be calculated online. To do so, a BMD measurement needs to performed prior to that.
- What is really increasing fracture risk in older people?
That's a tough question to answer. All we know for a fact is that fracture risk increases with age. And that risk factors exist that increase the risk of sustaining a fracture. But to which degree they play a part is still just speculation.
Though, it is likely a multimodal problem. Fall mechanics and protective mechanisms change and get slower as we age, so does bone quality (not just BMD). Less fat and muscle mass (as common in older people) provide less padding. There are surely other factors that play a part in increased fracture risk and all of them together will paint the big picture.
- When and why should you get your BMD checked?
It is recommended to check the BMD in people who (Morin et al., 2023):
a. are aged 50–64 yr with a previous osteoporosis-related fracture or ≥ 2 clinical risk factors OR
b. are aged ≥ 65 yr with 1 clinical risk factor for fracture OR
c. are aged ≥ 70 yr
And what are the clinical risk factors?
Previous fracture (after age 40), Falls (>2 in last year), BMI (of <20), Smoking, Alkohol (>3 drinks daily), Parent fractured hip, Glucocorticoids (>3 months), secondary osteoporosis.
What then?
After obtaining your BMD, your individual 10-year fracture risk will (or should) be assessed via FRAX (or some other calculator).
Depending on the calculated risk, you will be recommended initiating pharmacotherapy or not.
However, even if you are not recommended to initiate pharmacotherapy, you should get reassessed a couple years later (3-5 years) in order to see if something changed.
Exemplary patient:
A 60 year old patient with a 10 year fracture risk of <15% (or T-score of >-2.5) will usually not be recommended pharmacotherapy.
While a 75 year old patient with a fracture risk of >20% (or T-score of <-2.5) will benefit more from pharmacotherapy.
So it depends on the individual characteristics of each patient, whether medication is recommended or not.
However, each and every osteoprootic patient is recommended to perform balance and strengthening exercises (>2 times / week) in combination with a high calcium and protein diet, while supplementing Vitamin D (e.g. 400 IU daily).
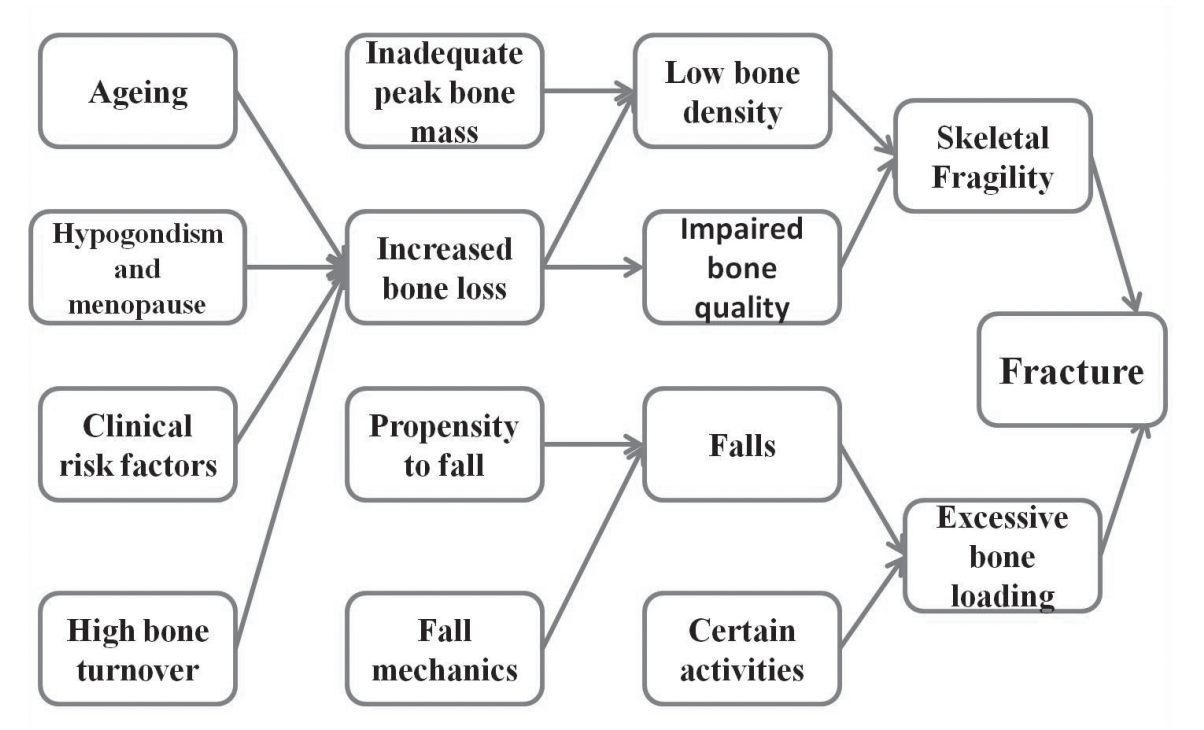
- Why do we develop osteoporosis?
A quick dive into physiology helps better understand this topic:
Bone is constantly being remodelled. Osteoclasts break tissues down (which is a necessary and important function, to keep bones healthy) and osteoclasts build it back up (to keep bone mass where it is).
This process starts at birth and accompanies us until adulthood.
Until we reach our peak bone mass (maximum amount of bone), the bone formation rate (osteoblastic activity) is greater than the bone resorption rate (osteoclastic activity).
Then (as it is with muscle mass and the development of sarcopenia) the balance between bone formation and resorption naturally shifts in favour of resorption, leading to a slow but certain reduction in bone mass.
As we age and factors such as menopause cause hormonal disturbances, the balance is shifted even further towards resorption and the chances of sustaining a fracture increases.
As shown in the figure from Weaver et al. below, the higher the peak bone mass, the slower the onset of osteoporosis (if one assumes a similar reduction across time between individuals). This process can be sped up or slowed down mainly via lifestyle choices, genetic factors or endocrine disorders. More on that below.
- Can we prevent it? does lifestyle matter? or is it simply genetics?
Osteoporosis is sometimes referred to as a pediatric condition with geriatric consequences. Meaning that the problem lies in the way we live during our youth / puberty, which then heavily affects our life as older adults.
This makes sense, as bone modelling is very sensitive to physical (or mechanical) stress, which makes a point for lifestyle factors such as exercise (especially in younger ages) to play an important part in the development of bone architecture.
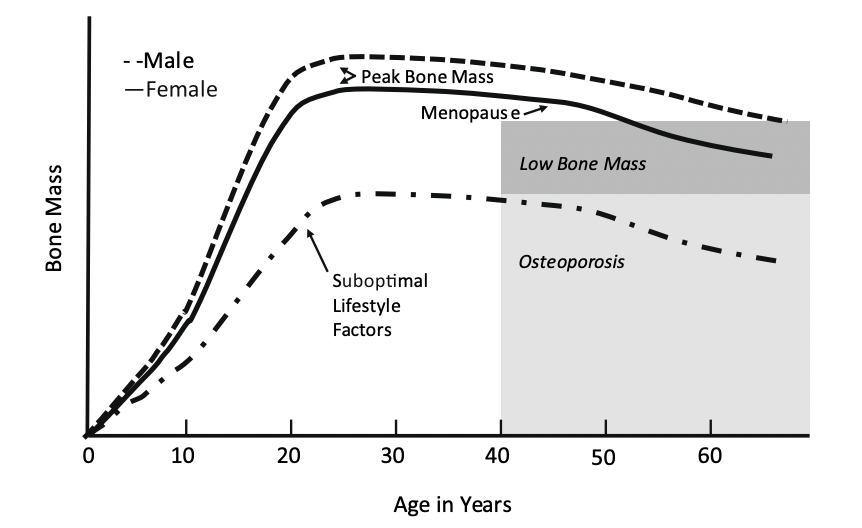
As the above figure beautifully illustrates, suboptimal lifestyle choices (especially during youth) can significally dampen maximal bone mass acquisition.
This means that adequate prevention of osteoporosis does not start after menopause (although there is still things you can do there), but in youngsters!
Especially around the 10-20 year time span (to be more precise: 12 years in girls and 14 years in boys, within +/- 4 years, are crucial). With high importance of the pre-pubertal years.
The authors of a systematic review on bone mass development stated that there is "strong evidence that bone status during childhood, when peak bone mass is accumulated, is indicative of bone status in young adulthood" and therefore "lifestyle factors can alter bone status in both positive and negative directions" (Weaver et al., 2016).
In the same study, gave level A graded evidence to only two out of all the factors they looked at: Calcium intake and physical activity, especially for peripubertal years. As during these years, bone development is critical and will be assisting a person throughout a lifetime. Having adolescents engage is sports such as soccer, ice hockey, basketball, volleyball... with high intensity impacts (e.g. jumps) applied at short duration (e.g. sprinting) in various planes of motion (e.g. change of direction), gives the bone lots of stimuli.
While these sports have plyometric exercises integrated and are therefore highly osteogenic. As (heavy) resistance training is also known to be osteogenic, it can be added to sports participation to improve BDM in adolescents. For example in distance runners it has been shown, that the addition of resistance training to their running can help increase BMD and is therefore recommended at least once weekly (Duplanty et al., 2018).
For other sports, finings are more nuanced. It is only natural to assume that some sports are more or less osteogenic than others. Running, as named above is a less osteogenic exercise (as it is too repetitive and easy to habituate to) and may therefore benefit from additional resistance exercise. This should also be true for cycling and swimming (sports with even less mechanical stimulation). This has been supported by a recent study performed on swimmers, where the addition of a resistance training regime resulted in beneficial increments in BMD (Agostinete et al., 2024). Although the study had its limitations, they found no added benefit of resistance training (RT) when looking at weight-bearing sports (basketball, tennis, gymnastics). This might be due to the "ceiling effect" where these sports are already pushing bone mass accumulation to the limit, where additional input does not seem to change the game, or due to these kids having a higher stimulation threshold needed to achieve adaptation from RT. Similar findings have been found in another trial, where a 9-month jumping intervention resulted in improved BMD in swimmers and cyclists, but not in footballers (Vlachopoulos et al., 2018).
Therefore, it is likely the case that the more osteogenic a sport is, the less the participants will benefit from additional RT or plyometric exercise. At least in adolescents.
Some sports and their osteogenic potential:

- What about running? is that not enough for lower limb BMD?
A landmark paper from Robling and colleagues from 2002 (though performed on rats) provided initial evidence that exercises should be provided across different bouts, meaning that rest periods should be included instead of getting it all done in one series (Robling et al., 2002).
It seems as this paper has often been used as an argument against running for the development of BMD or bone strength, due to it being an exercise performed in one go after any rest in between. This would make a natural point for interval training to be more osteogenic than running. Whether that's true of not is hard to tell, as interval training is characterised by higher training intensity, which makes comparisons difficult. Then should one add breaks to normal running? to provide the bone with adequate stimuli? Maybe.
If the argument against running is true (by being a less osteogenic exercise type) it is not irrational to assume that it is due to the shortness of impacts, that might be too quick to initiate mechanotransduction. Just as it is the case with tendons, where tendinopathies respond better to heavy resistance training if the goal is to increase tendon stiffness, rather than plyometric exercise.
But, when it comes to bones, plyometric exercise actually are seen as a very anabolic stimulus for the bone. Especially in young athletes, where sports such as soccer, basketball... with short sprinting bouts and lots of changes of direction sort of movements, are seen as some of the best sports for children when it comes to the development of BMD.
Where does that leave us? It might be a combination of factors, such as intensity of running that is not high enough or the duration of loading too short that makes it less osteogenic. In fact, we simply do not yet know. Some papers are finding contradicting results. As some speculate that the discrepancies in findings is due to the population we are looking at. Being long distance runners. As these people are prone towards energy deficiencies (e.g. female athlete triad; RED-S), which impacts anabolism of the body, creating a less than optimal environment for BMD development. A cohort study found that when correcting for low energy availability, runners with high energy availability have increased BMD compared to non-running controls. They concluded that "in male collegiate runners, the weight-bearing activity provides a beneficial effect in BMD at the hip, femoral neck, and whole body" (McCormack et al., 2019).
While another study, cross-sectional, found that "a high level of sport specialization in high school female distance runners may be associated with a heightened risk for low BMD" (Rauh et al., 2020), but they also found an association between high levels of specialization and menstrual dysfunction. And they did not check for energy availability, as they did in the study cited above. Making these findings less about running and more about the female athlete triad.
- What can we do to reduce fracture risk?
When we are talking at the prevention of osteoporotic fractures, most of the literature has looked at how to do so for postmenopausal women. Which of course, is a very relevant topic, as women are more affected by osteoporosis than men.
So, what can middle-aged women do about it?
First of all we need to be aware of the problem, before we think about preventing it. What do we want to prevent? Well, obviously we want to keep BMD high. But the real problem with osteoporosis is increased risk of fracture. And unless your osteoporosis has advanced to levels where spontaneous fractures can occur (which is rare), the way you fracture a bone is from falling.
This leads us to 2 sub-questions: how do we effectively increase BMD? and decrease fall incidence in middle-aged women?
Falls are associated with decreased muscle strength, muscle power, balance, slow walking speed... making exercise a keystone intervention for that.
For BMD, we need to be more body part specific. Most fractures occur at the hip, spine and wrist. And as high impact jumps sadly won't affect wrist BMD, a full body workout program should be implemented.
Bone has been shown to quickly adapt to continuing stimuli, which makes progressive overload a key training principle for individuals seeking to improve bone mass.
Regarding training duration, the authors of a review on training recommendations for postmenopausal women, stated that: "the response time of bone to loading is slow because the typical bone remodelling cycle lasts 3 to 8 months. Thus interventions must last a minimum of 6 to 9 months (preferably 12 to 24 months) to detect any measurable or ‘true’ physiological skeletal changes beyond the normal bone remodelling transient". As well as "the mechanosensitivity of bone diminishes with age and any exercise-induced changes in bone density after menopause are typically modest (1—3%)" (Daly et al., 2019), which seems like nothing but has been shown to be enough to reduce fracture risk from falls.
A combination of progressive resistance training (with progressions towards power training), balance training (including rapid stepping exercises) and weight-bearing impact exercises (e.g. jumps) are recommended for a thorough training program to prevent osteoporosis for postmenopausal women (Daly et al., 2019).
For older individuals, a thorough education about general precautions such as removing unnecessary carpets (stumble danger), turning the lights on at night (going to the bathrooms with light on can lead to unnecessary falls), putting on the glasses and good fitting shoes.
- Does nutrition play a role?
In general, eating a balanced diet will give you most of the nutritional benefits regarding fracture risk.
If you eat enough protein (>0.8g/kg) and calcium (>1000 or >1200 mg/day for males / females) rich foods, while supplementing vitamin D (400 IU) on a daily basis for adults > 50 years old (Morin et al., 2023), you are good to go.
But make sure you are getting enough food in. As "in particular protein and caloric under-nutrition, are considered fracture risks by impairing muscle strength and function, thereby increasing the risk of falling" (Pinto et al., 2022).
- Is osteoporosis reversible?
For osteoporosis to be reversible, it would mean that a therapeutic intervention had to increase bone density and bone mass substantially. Such a treatment does not yet exist. Pharmacological interventions (e.g. biphosphonates) help reduce osteoclastic activity and thereby reduce further bone loss (with a reported increase in BMD of 2-5%). While exercise interventions, such as resistance training, also mainly prevent further bone loss (and maybe increase BMD by 1-2%).
Therefore we cannot yet say that we can reverse osteoporosis.
- ”I was diagnosed with osteoporosis, can I continue running?"
In older people, pain from osteoarthritis, severe osteoporosis and a recent history of fracture might contraindicate impact exercises such as running. But is this true for everyone?
The recent Canadian clinical practice guidelines express uncertainty regarding their recommendations for impact exercises: "safety or efficacy of impact exercise is uncertain in people at high fracture risk (e.g., history of spine fracture or 10-yr fracture risk for major osteoporotic fracture of ≥ 20% )" (Morin et al., 2023).
Which leads us to an individual case by case approach. People who have been running their whole life and are not categorised as having high risk of fracture are probably fine continuing running even after getting osteoporosis.
While other people, also not in the high risk category, but haven't been running for a long time and want to start again, for those people a more slow and progressive approach towards running (with initial jumping progressions...) needs to be implemented.
- What's the "best'' intervention for osteoporosis/-penia (resistance training, balance, walking, running, combined?)
In order to decide which exercise ist "best", we need first decide which particular bone we are looking at. As the adaptation in bone mineral density (BMD) of various bones reacts differently to different exercises.
A recent network meta-analysis aimed at discriminating exercise efficacy between lumbar spine, total hip and femoral neck BMD increases. They found that for the lumbar spine, aerobic, resistance training, combined (resistance training + aerobic) and mind-body exercise was showing significant improvements with mind-body exercise eliciting the greatest improvements.
For the femoral neck, all exercise types showed improvements, but once again mind-body exercise led to the most prominent ones.
Whereas for total hip, only resistance training and aerobic exercise led to improvements in BMD, with resistance training outranking aerobic exercise (Zhang et al., 2022).
Mind-body exercises include Thai Chi and Qigong and are characterised by slow, controlled and rhythmic movements. The continuous half-squatting stance adopted by these practices likely adds to the positive adaptations seen when studying its effects. Therefore, mind-body exercises are recommended, as they are effective and due to their "slow-moving" nature, safe for older populations aiming to improve lumbar- and femoral bone health (but not for the hip).
Aerobic exercise included walking and brisk walking (although the efficacy of simple walking is critically discussed in the literature). Aerobic exercise has been shown to increase BMD in all 3 areas, but to a lesser degree than other interventions, but is a good way to get moving for the elderly.
Resistance training has been ranking second place after mind-body interventions, though with contradicting evidence for the efficacy of lumbar spine BMD increases.
Regarding this network meta-analysis the authors stated in their limitations that there was a high risk of bias in the included studies (as 2/3 of them were performed in china) which might explain some effects of the mind-body interventions for BMD, but regarding balance and therefore reduced fall-risk it makes sense to include these exercises.
Practical implications:
- Full body resistance training combined with brisk walking (or running / jumping) increases BMI in all bones and is recommended for more active populations.
- Mind-body exercises should be complemented with resistance training (for the total hip bone) and can be recommended for every age group.
- Why exercise for osteoporosis?
When taking a closer look on the evidence behind BMD and exercise, we see that the increases in bone mass from exercise in older people are small. Although the authors of a systematic review on the topic attributed the small effect sizes to the large heterogenity in exercise protocols, with some finding way better outcomes than others (Shojaa et al., 2020).
As our population further develops, people get older and older and our bones are going to continue to deteriorate. Therefore, spontaneous fractures will be more frequent, and less forceful impact will be needed to cause severe disability.
Therefore, even if increases in BMD are small according to research, is is pretty clear that BMD loss can be slowed down. Which might be even more important looking forward.
How can exercise be made more effective?
Progressions: Exercises need to be progressed over time to continually provide adequate strain to the bones.
Duration: Exercise participation should be sustained for longer periods. Several months (>8) of training are recommended, considering bone remodelling time periods.
Intensity: High intensity >70%1RM is recommended (very old and highly osteoporotic people might want to start at lower intensities, 40-50% 1RM, and work their way up). In line with previous recommendations, we suggest that resistance training should progress to high intensity. While some recent meta-analyses have not found significantly greater benefits from high-load compared to lower-load resistance exercises, the progression to higher intensity remains advisable (Brooke-Wavell et al., 2022).
Repetitions: The higher the intensity (or strain for bones) the less repetitions are needed. But if less strain is applied, more loading cycles may make up for it. So, go heavy with few reps if possible, and when that type of training is not possible, reduce load and increase repetitions.
According to another recent systematic review, it does not matter whether exercise is supervised or unsupervised, as long at intensity is progressed over time (Mohebbi et al., 2023).
Regarding everything else, progressing over time seems to be key, as "strain has to be steadily increased and/or modified to account for bone familiarization and so generate continuous adaptation" (Kemmler & Von Stengel, 2019).
- Can we alter falling mechanics to reduce fracture risk?
Another strategy to reduce fracture risk (especially at the hip) is by tearching the elderly how to fall. This intervention been performed in a couple of studies, looking at Martials Arts (MA) fall technique (more of a rolling off movement) and how impact forces at the hip changed after being trained in MA falling technique. And the studies reported significant reductions in impact forces, stating that "rolling on after hip impact may indeed play an important role in the reduction of hip impact force" (Groen et al., 2010).
And another good think of fall training is that fear of falls can be reduced by such interventions. Which is logical, as constant exposure to falls in a safe environment will ultimately reduce anxiety towards that very thing. This has been shown after only 5 sessions of 30 min training. Such an intervention might be especially effective in those with a high fear of falling.
- What are the dangers of sustaining an osteoporotic fracture?
Around one-third of those sustaining a hip fracture, die within 1 year. Therefore, osteoporotic fractures should not be taken likely.
As we have seen, exercise is important for the prevention of fractures, and that's true also for re-fracture rates. A recent systematic review and meta-analysis found that in people with osteoporotic fractures, "after a fracture, timely and systematically providing exercise therapy intervention reduced the incidence of refractures after three years by 3.67 times compared to patients who did not receive exercise therapy" (Yu et al., 2025). These effects can likely be explained via the same mechanisms as for those without a fracture. Increases in BMD and reduction in fall risk.
In general, hip fractures benefit a lot in terms of regaining functionality when a resistance training program is commenced 3-6 months after the fracture / surgery. As improvements in strength, balance, walking speed... (Soro-García & González-Gálvez, 2025).
- Are there movements that I should not do with osteoporosis?
Osteoporotic fractures may be caused by a fall or with loading during activity. People with osteoporosis and health professionals are thus concerned that physical activity could increase fracture risk, although evidence to support these concerns is limited. Uncertainty persists about what is appropriate and safe in people with osteoporosis and as a result, people significantly reduce activity levels, limiting both function and enjoyment. This may have important adverse implications for their bone health, falls and future fracture risk.
Overall, intervention group participants sustaine less fractures compared with control group participants. Closely supervised high-intensity resistance and impact training in osteoporotic men and women was associated with few adverse effects and no vertebral fractures (Kunutsor et al., 2018).
Fracture risk is only higher when people are moving from one place to another (risk of falls), but overall, there is little evidence of harm, including fractures, occurring while exercising (controlled environment). Exercise is therefore unlikely to cause a fracture (and specifically a vertebral fracture) and does not need to be adapted for those with osteoporosis according to fracture risk or low BMD. Safe lifting techniques are recommended rather than instructions such as ‘don’t lift’ or ‘only lift up to a specific weight’. Furtheremore rotation (twisting) movements should be safe if performed smoothly and comfortably (Brooke-Wavell et al., 2022).
The only thing to be cautious: Movements or exercise that involve sustained, repeated or end- range flexion should be modified or avoided. Any exercise that causes the back to curve excessively especially with an added load should be modified or avoided. But for people who are experienced, demonstrate flexibility in the spine and can manage the moves comfortably and smoothly, should be advised that they can continue with these activities as long as they are fit enough to manage them with ease. As said, people with osteoporosis should be encouraged to do more rather than less, as there is little evidence that physical activity is associated with significant harm, and the benefits, in general, outweigh the risks (Brooke-Wavell et al., 2022).
- Can we give every person with osteoporosis the same exercise protocol?
Absolutely not.
There is a strong need for individualising exercise programs for osteoporosis management. This has to do with the different risk factors that people present with, and with the bone site we are trying to manage. Although they will each get a mix of balance and strengthening exercises, the ratio of those exercises (more strengthening and less balance or the other way around) depends on the individual presentation of the patient.
This is easily understood when looking at two different populations:
Population A: Early postmenopausal women usually do not have any postural control issues, making an emphasis on balance training (for fall prevention) less important. But they do have increased bone turnover, making strengthening and impact exercises a way better choice for this population.
Population B: A fragile old man with a history of vertebral fractures and at high fracture risk (FRAX), will probably have to reduce strengthening (especially in the end ranges of the spine) and increase the focus of fall prevention (e.g. balance training).
- What does an appropriate exercise selection for osteoporotic patients look like?
Resistance Exercises:
Aims at: increasing (or decrease loss of) bone mass and fall prevention. Exercises should be selected to specifically target the clinically relevant sites. As bone adaptation is specific to the site of mechanical strain. Compound movements are a good choice for that.
The literature suggests that resistance training performed as a single intervention, or combined with other forms of physical activity "may be the most optimal strategy to improve the muscle and bone mass in postmenopausal women, middle-aged men, or even the older population"(Hong & Kim, 2018).
Highly osteoporotic patients can start at 40-50% 1RM, but working up towards 70%-85% is recommended
How much?
2-3 x / week, 8-10 exercises with 2-3 sets and 5-12 reps each; 1-3 minutes rest
- Squat pattern, Hinge pattern, Pulling, Pushing, Step-ups
Weird extra: tibialis anterior raises -> as older people often fall backwards, and raising the forefoot helps balance in the sagittal plane.
Avoid loaded spinal flexion in those with previous vertebral fractures.
Is is also recommended that "as soon as subjects are able to carry out the exercise safely, i.e. with proper biomechanical execution, movements must be performed focusing on achieving the maximal execution speed possible", as explosive movements are said to be especially osteogenic (Guadalupe-Grau et al., 2009).
Caution with spine bending and twisting in those with vertebral fractures and low spine BMD.
Impact exercises:
Aims at: increasing bone mass at the lower extremity (proximal femur). Not so much at the lumbar spine.
Start at around 10 jumps per session and progress towards 50 jumps / session.
- Jumping progressions, Hopping, Running, jump rope, jumping chin-ups with drop landing
How much?
3 x / week for 50 reps total
5 sets of 1-10 reps, 1-2 min rest per set
Balance training:
Aims at: reducing fall risk
- Dynamic balance: heel / toe walking, walking in one line, walking backwards, Tai chi, dance, yoga
- Static balance: Single leg stance, tandem foot standing, weight shifting
Variables: Vision, speed and head movements can be included to manipulate exercise difficulty.
Start static and progress towards dynamic movements.
How much?
3 x / week (up to daily) for 20-40 min per session (a total of 2h per week)
Integrating balance exercise: Balance training can be performed daily (with 2h of weekly volume being recommended). To do so without taking up valuable free time, we can recommend integrating balance exercises into activities of daily living. Such as standing in tandem while washing the dishes or performing a single leg stance while brushing ones teeth. This approach has been shown to lead to the same outcomes than a structured training program, when it comes to falling incidence in the elderly (Clemson et al., 2012).
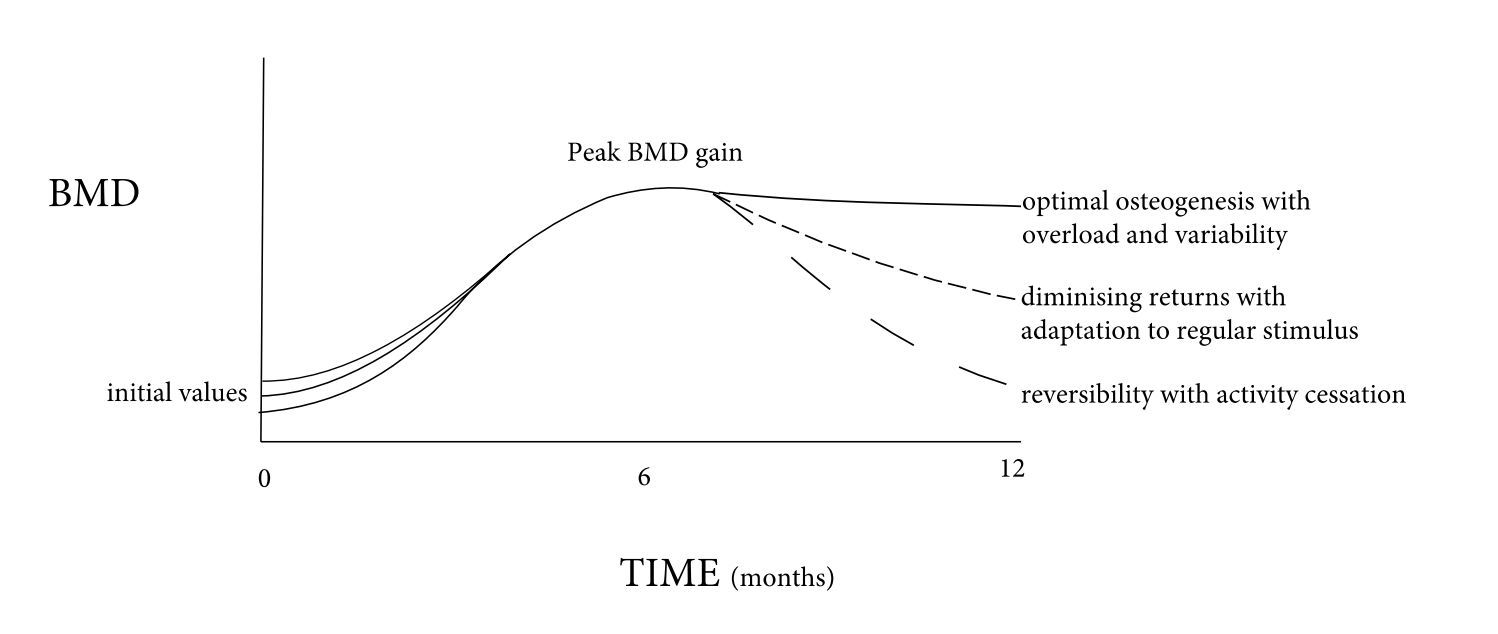
General principles of mechanical loading on BMD adaptation:
- Input needs to vary and be constantly progressed
- Once the bone is accustomed to an intervention, returns diminish
- Cessation of exercise will reverse the made improvements in time
Therapeutic conclusion:
A combination of resistance and balance exercise will be your best bet. As the authors of a recent clinical practice guideline stated "fall prevention by improving postural balance may be more important than the effect of exercise on BMD in terms of fracture" and that the "most effective fall-prevention exercise programs have yet to be clarified, but programs targeting strength and balance appear particularly effective" (Bae et al., 2023).
- What about training with / after vertebral fractures?
For people with vertebral fractures, no strong guidelines exist, on which exercises are safe to perform and wich are not. In general, researchers recommend " slow, controlled movements" for this population. While they point out the "importance of including exercises targeting muscles important for posture (e.g., spinal extensor muscles), and that individuals with osteoporosis or vertebral fracture are educated about proper posture during exercise and every day activities" (Giangregorio et al., 2014). What this proper posture looks like is not described, but likely recommends a "neutral" position, avoiding the end ranges of spinal flexion, especially in combination with rotation. At least, that is what the author of the above paper, and osteoporosis expert Laura Giangregorio recommended in a podcast episode (see below). Resistance training is nontheless recommended and encouraged in this population. A recent narrative review stated to refraim from activities that "involve rapid, repetitive, weighted, or end-range twisting or flexion of the spine, or that have high fall risk" (Pinto et al., 2022).
Vertebral fractures also come with changes in posture and oftentimes decreases in balance. Something to look out for.
- Do higher training loads lead to greater bone adaptations?
Generally it is believed, that high training loads are needed to generate the best outcomes. This is not quite true. What is true, is that exercise needs to be PROGRESSED. At whichever weight / intensity you start at, you do so and you will be seeing benefits, even going as low as 40% 1RM has been reported (Souza et al., 2020). As usual recommendations are to work your way up towards higher 1RM percentages (>70%), it seems staying in the lower ranges can still be beneficial (as long as effort is high enough), but progressions still need to happen. And the same authors concluded that higher load RT might be more effective for those with higher BMD. Suggesting that people with lower BMD respond better to lower intensity training, which makes logical sense.
Others studies support this conclusion. As the LIFTMOR trial found additional benefits from combining heavy resistance training with impact exercise, which means that intensity does matter, while being a safe intervention for women with low- to very-low BMD (Watson et al., 2018).
One could argue that impact exercises played the more important part here and that RT intensity did not quite matter as much. Maybe. But as strength training acts via two pathways (mechanical stress on the bone from the muscular pull) and hormonal responses (via myokines) the mechanical stress increases with intensity. Therefore we recommend you to go as heavy as possible, while still being safe and comfortable.
Adaptations in bone structure is determined by the magnitude and rate of mechanical loading. And a minimum threshold needs to be reached for mechanotransduction to start off. In non-physically active people, such loads would need to be greater than what they experience during activities of daily living. But once people start "lifting" bone will adapt to that as well and exercises will need to be progressed over time.
References:
Agostinete, R. R., Werneck, A. O., Narciso, P. H., Ubago-Guisado, E., Coelho-e-Silva, M. J., Bielemann, R. M., Gobbo, L. A., Lynch, B. T., Fernandes, R. A., & Vlachopoulos, D. (2024). Resistance training presents beneficial effects on bone development of adolescents engaged in swimming but not in impact sports: ABCD Growth Study. BMC Pediatrics, 24, 247. https://doi.org/10.1186/s12887-024-04634-0https://doi.org/10.1111/jocn.16101
Bae, S., Lee, S., Park, H., Ju, Y., Min, S.-K., Cho, J., Kim, H., Ha, Y.-C., Rhee, Y., Kim, Y.-P., & Kim, C. (2023). Position Statement: Exercise Guidelines for Osteoporosis Management and Fall Prevention in Osteoporosis Patients. Journal of Bone Metabolism, 30(2), 149–165. https://doi.org/10.11005/jbm.2023.30.2.149
Bouxsein, M. L. (2003). Bone quality: Where do we go from here? Osteoporosis International, 14(0), 118–127. https://doi.org/10.1007/s00198-003-1489-x
Brooke-Wavell, K., Skelton, D. A., Barker, K. L., Clark, E. M., De Biase, S., Arnold, S., Paskins, Z., Robinson, K. R., Lewis, R. M., Tobias, J. H., Ward, K. A., Whitney, J. & Leyland, S. (2022). Strong, steady and straight: UK consensus statement on physical activity and exercise for osteoporosis. British Journal Of Sports Medicine, 56(15), 837–846. https://doi.org/10.1136/bjsports-2021-104634
Clemson, L., Fiatarone Singh, M. A., Bundy, A., Cumming, R. G., Manollaras, K., O’Loughlin, P., & Black, D. (2012). Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): Randomised parallel trial. BMJ (Clinical Research Ed.), 345, e4547. https://doi.org/10.1136/bmj.e4547
Daly, R. M., Dalla Via, J., Duckham, R. L., Fraser, S. F., & Helge, E. W. (2019). Exercise for the prevention of osteoporosis in postmenopausal women: An evidence-based guide to the optimal prescription. Brazilian Journal of Physical Therapy, 23(2), 170–180. https://doi.org/10.1016/j.bjpt.2018.11.011
Duplanty, A. A., Levitt, D. E., Hill, D. W., McFarlin, B. K., DiMarco, N. M., & Vingren, J. L. (2018). Resistance Training Is Associated With Higher Bone Mineral Density Among Young Adult Male Distance Runners Independent of Physiological Factors. Journal of Strength and Conditioning Research, 32(6), 1594–1600. https://doi.org/10.1519/JSC.0000000000002504
Giangregorio, L. M., Papaioannou, A., Macintyre, N. J., Ashe, M. C., Heinonen, A., Shipp, K., Wark, J., McGill, S., Keller, H., Jain, R., Laprade, J., & Cheung, A. M. (2014). Too Fit To Fracture: Exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture. Osteoporosis International: A Journal Established as Result of Cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 25(3), 821–835. https://doi.org/10.1007/s00198-013-2523-2
Groen, B. E., Smulders, E., De Kam, D., Duysens, J., & Weerdesteyn, V. (2010). Martial arts fall training to prevent hip fractures in the elderly. Osteoporosis International, 21(2), 215–221. https://doi.org/10.1007/s00198-009-0934-x
Hong, A. R., & Kim, S. W. (2018). Effects of Resistance Exercise on Bone Health. Endocrinology and Metabolism, 33(4), 435–444. https://doi.org/10.3803/EnM.2018.33.4.435
Kemmler, W., & Von Stengel, S. (2019). The Role of Exercise on Fracture Reduction and Bone Strengthening. In Muscle and Exercise Physiology (pp. 433–455). Elsevier. https://doi.org/10.1016/B978-0-12-814593-7.00020-7
Kunutsor, S. K., Leyland, S., Skelton, D. A., James, L., Cox, M., Gibbons, N., Whitney, J. & Clark, E. M. (2018). Adverse events and safety issues associated with physical activity and exercise for adults with osteoporosis and osteopenia: A systematic review of observational studies and an updated review of interventional studies. Journal Of Frailty Sarcopenia And Falls, 03(04), 155–178. https://doi.org/10.22540/jfsf-03-155
McCormack, W. P., Shoepe, T. C., LaBrie, J., & Almstedt, H. C. (2019). Bone mineral density, energy availability, and dietary restraint in collegiate cross-country runners and non-running controls. European Journal of Applied Physiology, 119(8), 1747–1756. https://doi.org/10.1007/s00421-019-04164-z
Mohebbi, R., Shojaa, M., Kohl, M., Von Stengel, S., Jakob, F., Kerschan-Schindl, K., Lange, U., Peters, S., Thomasius, F., Uder, M., & Kemmler, W. (2023). Exercise training and bone mineral density in postmenopausal women: An updated systematic review and meta-analysis of intervention studies with emphasis on potential moderators. Osteoporosis International, 34(7), 1145–1178. https://doi.org/10.1007/s00198-023-06682-1
Morin, S. N., Feldman, S., Funnell, L., Giangregorio, L., Kim, S., McDonald-Blumer, H., Santesso, N., Ridout, R., Ward, W., Ashe, M. C., Bardai, Z., Bartley, J., Binkley, N., Burrell, S., Butt, D., Cadarette, S. M., Cheung, A. M., Chilibeck, P., Dunn, S., … Wark, J. D. (2023). Clinical practice guideline for management of osteoporosis and fracture prevention in Canada: 2023 update. Canadian Medical Association Journal, 195(39), E1333–E1348. https://doi.org/10.1503/cmaj.221647
Pinto, D., Alshahrani, M., Chapurlat, R., Chevalley, T., Dennison, E., Camargos, B. M., Papaioannou, A., Silverman, S., Kaux, J.-F., Lane, N. E., Morales Torres, J., Paccou, J., Rizzoli, R., Bruyere, O., & Rehabilitation Working Group of IOF Committee of Scientific Advisors. (2022). The global approach to rehabilitation following an osteoporotic fragility fracture: A review of the rehabilitation working group of the International Osteoporosis Foundation (IOF) committee of scientific advisors. Osteoporosis International: A Journal Established as Result of Cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 33(3), 527–540. https://doi.org/10.1007/s00198-021-06240-7
Rauh, M. J., Tenforde, A. S., Barrack, M. T., Rosenthal, M. D., & Nichols, J. F. (2020). Sport Specialization and Low Bone Mineral Density in Female High School Distance Runners. Journal of Athletic Training, 55(12), 1239–1246. https://doi.org/10.4085/1062-6050-0547.19
Robling, A. G., Hinant, F. M., Burr, D. B., & Turner, C. H. (2002). Improved bone structure and strength after long-term mechanical loading is greatest if loading is separated into short bouts. Journal of Bone and Mineral Research: The Official Journal of the American Society for Bone and Mineral Research, 17(8), 1545–1554. https://doi.org/10.1359/jbmr.2002.17.8.1545
Sangondimath, G., Sen, R. K. & T, F. R. (2023). DEXA and Imaging in Osteoporosis. Indian Journal Of Orthopaedics, 57(S1), 82–93. https://doi.org/10.1007/s43465-023-01059-2
Shojaa, M., Von Stengel, S., Schoene, D., Kohl, M., Barone, G., Bragonzoni, L., Dallolio, L., Marini, S., Murphy, M. H., Stephenson, A., Mänty, M., Julin, M., Risto, T., & Kemmler, W. (2020). Effect of Exercise Training on Bone Mineral Density in Post-menopausal Women: A Systematic Review and Meta-Analysis of Intervention Studies. Frontiers in Physiology, 11, 652. https://doi.org/10.3389/fphys.2020.00652
Soro-García, P., & González-Gálvez, N. (2025). Effects of Progressive Resistance Training After Hip Fracture: A Systematic Review. Journal of Functional Morphology and Kinesiology, 10(1), Article 1. https://doi.org/10.3390/jfmk10010054
Sozen, T., Ozisik, L., & Calik Basaran, N. (2017). An overview and management of osteoporosis. European Journal of Rheumatology, 4(1), 46–56. https://doi.org/10.5152/eurjrheum.2016.048
Vlachopoulos, D., Barker, A. R., Ubago-Guisado, E., Williams, C. A., & Gracia-Marco, L. (2018). A 9-Month Jumping Intervention to Improve Bone Geometry in Adolescent Male Athletes. Medicine and Science in Sports and Exercise, 50(12), 2544–2554. https://doi.org/10.1249/MSS.0000000000001719
Watson, S. L., Weeks, B. K., Weis, L. J., Harding, A. T., Horan, S. A., & Beck, B. R. (2018). High-Intensity Resistance and Impact Training Improves Bone Mineral Density and Physical Function in Postmenopausal Women With Osteopenia and Osteoporosis: The LIFTMOR Randomized Controlled Trial. Journal of Bone and Mineral Research, 33(2), 211–220. https://doi.org/10.1002/jbmr.3284
Weaver, C. M., Gordon, C. M., Janz, K. F., Kalkwarf, H. J., Lappe, J. M., Lewis, R., O’Karma, M., Wallace, T. C., & Zemel, B. S. (2016). The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: A systematic review and implementation recommendations. Osteoporosis International, 27(4), 1281–1386. https://doi.org/10.1007/s00198-015-3440-3
Yu, M., Zhou, P., Che, Y., & Luo, Y. (2025). The efficacy of exercise prescription in patients with osteoporotic fractures: A systematic review and meta-analysis. Journal of Orthopaedic Surgery and Research, 20(1), 250. https://doi.org/10.1186/s13018-025-05636-z
Zhang, S., Huang, X., Zhao, X., Li, B., Cai, Y., Liang, X., & Wan, Q. (2022). Effect of exercise on bone mineral density among patients with osteoporosis and osteopenia: A systematic review and network meta‐analysis. Journal of Clinical Nursing, 31(15–16), 2100–2111. https://doi.org/10.1111/jocn.16101