Section C: Bone Stress injuries

Diagnosis:
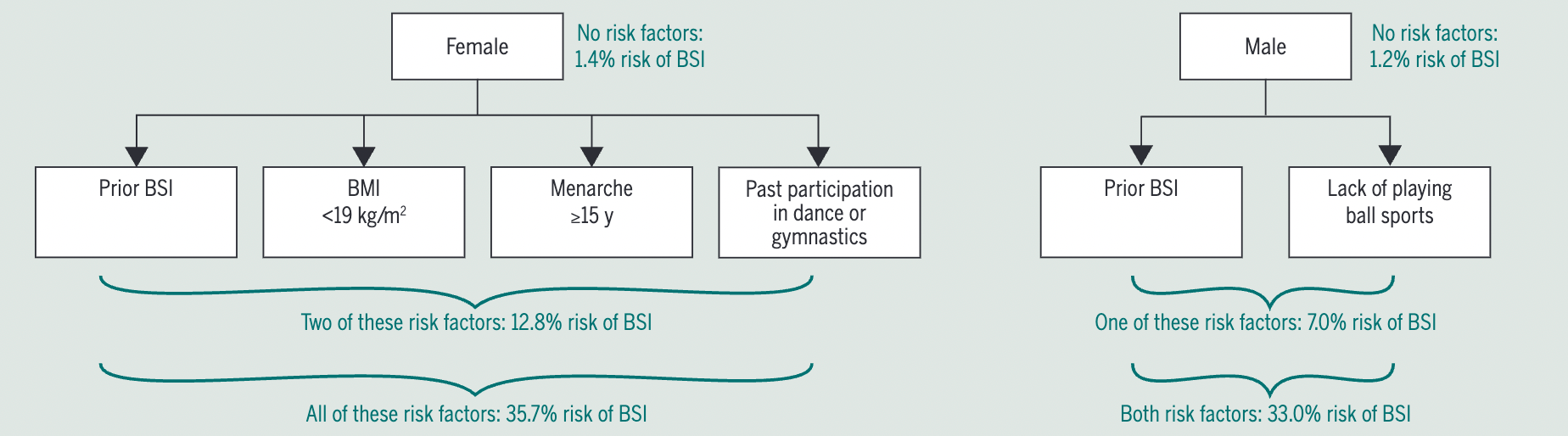
Diagnosis is achieved by a combination of patient history and physical examination, with imaging used for confirmation and to grade the injury and guide management. Suspicion is raised in the presence of key risk factors including participation in an ‘at risk’ activity, whether the individual has a history of a previous bone stress injury, their physical activity levels and the presence of indicators of REDs.
Step 1: Detailed Patient History
Look for clues that raise suspicion:
- Recent increase in activity (especially in past 4–6 weeks)
- Participation in long distance running
- Signs of RED-S or female athlete triad (more information on those below)
Step 2: Symptoms
- Pain with activity that worsens with loading (usually no warm-up phenomenon)
- Pain subsides with rest
- In more advanced cases, pain may persist at rest or at night
- No obvious traumatic event
- Pain is initially diffuse, but becomes better localised as the condition progresses
Step 3: Physical Examination
- Localized tenderness over the affected bone (especially subcutaneous bones like tibia or metatarsals)
- Pain with hopping on the affected leg (for lower limb), especially important for bones that can not be palpated
- Special tests for deeper injuries:Fulcrum test for femurSqueeze test for calcaneus
Pain is the most important diagnostic feature on physical examination. Although they may vary in symptoms, most bone stress injuries are normally pain free when unloaded and worsen with increased load, but advanced bone stress injuries can be painful at rest, including at night. This is a continuum: Initially, pain is mild, diffuse, and appears only during specific parts of the running gait. It doesn't improve with continued running but stops once the run ends, so it's often ignored. As the condition worsens with continued training, the pain becomes more severe, localized, starts earlier, and lasts longer after running. Eventually, it may appear during less intense activities like walking and could lead to stopping training altogether. In advanced stages, inflammation may also cause pain at rest or at night (Hoenig et al., 2022).
Step 4: Imaging / Classification
Imaging is used for confirmation, to grade the injury and guide management.
The current best choice indicated by research and expert consensus is MRI (Wright et al., 2015; Hoenig et al., 2024).
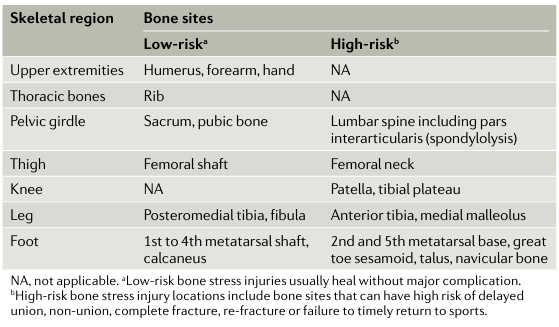
In addition to classifying a BSI as either low or high risk according to anatomical location, a BSI can be categorized as either low or high grade according to its imaging appearance (severity of injury) (Warden et al., 2014). So The current best practice system for classifying low or high grade injuries are by Fredericson et al. (1995) which uses MRI imaging (Hoenig et al., 2024).
- Low-risk BSIs:
- Occur on the compression side of the bone.
- Typically heal well with minimal intervention.
- Have a faster recovery and lower complication risk.
- High-risk BSIs:
- Occur on the tension side of the bone.
- More prone to delayed healing, nonunion, or full fractures.
- Require careful management and longer recovery.
- Low-grade (Grade 1–2):
- Represent early-stage injuries with shorter recovery (about 13 weeks).
- High-grade (Grade 3–4):
- More advanced and take longer to heal (about 24 weeks)
Combining location and grade helps predict recovery time and guides treatment.
- Low-risk + low-grade = quickest recovery
- Low-risk + high-grade = longer recovery
- High-risk (any grade) = longest recovery and needs close monitoring
The grading with MRI and therefore the injury management is solely recommended if the patient describes and shows clear symptoms of a bone stress injury. If not, imaging to identify presymptomatic BSI are of no clinical value (Warden et al., 2014).

How do BSIs develop?
Exercise, especially with heavy impacts, can lead to micro-damages in bone tissue. This leads to bone remodelling. Osteoclasts are activated to remove damaged bone at the site of injury and afterwards osteoblasts build new bone in that same spot to make it more resistance for future impacts (after being activated by mechanosensitive osteocytes). This process is normal and highly important (especially in adolescents) for peak bone mass development. Therefore, microdamage is necessary for bone adaptation. Mechanical loading increases osteoblastic activity, while partly inhibiting osteoclastic activity, leading to a net increase in bone mass.
As we found out in Section A, a lack of such stimulation leads to decreases in bone mass and problems down the road. While too much of a mechanical stimulus (especially from external impacts) leads to bones cracking down (fracture).
But there is something in between these two spectrums. It's when people are active enough to mechanically stimulate bone, but the impacts are not strong enough to lead to a fracture and are therefore repeated over and over again. At some point, the bone remodelling shifts away from "building stronger bones" towards "accumulated micro-damages" that now evolve into macro-damages we call bone stress injuries. So, in BSIs the bones ability to heal itself is outweighed by the stressors of cumulative loading. While in a healthy athlete, we can assume that new microdamage only forms after old microdamage has been removed.
Management differences between high-risk and low-risk BSIs
All BSIs are believed to heal from bone remodelling.
Management of low-risk BSIs: (Warden et al., 2021a)
- Load management:
The first stage of management is made up of activity modification.
Pain during, immediately after or the day after activity needs to be avoided, as it might delay healing. A period of non-weight bearing is not normally indicated in these people.
Achieving a pain free gait is an important goal (and might only be possible with crutches or a cane, often in combination with cushioned shoes for tibial BSIs or stiff soled shoes in those with metatarsal BSIs).
In some, a change in footwear will be enough, while others might be experiencing higher levels of pain and require a non-weight bearing (crutches) or walking boot intervention. . When pain is present during night time, it is an indicator of an inflammatory component and NSAIDs might be considered (for a maximum of a few days).
In general: reduce exercises to a level where exercising is pain free (with no pain after) and modify ADLs (by using cushioned shoes, stiff-soled shoes, crutches... depending on site and severity of BSI) to allow for tissue healing. Typically, low-risk BSIs heal without further complications, when adhering to these principles.
- Maintain fitness:
To reduce losses in cardiovascular fitness, cross training should be commenced (swimming / riding a bicycle / deep water running / antigravity treadmill). This should be done without provocation of symptoms (antigravity running should be done only after being pain-free during ADLs and with walking for a week). During this time, make sure to screen for RED-s (and if needed refer to a clinician). In the case of energy deficiency, educate them about the importance of providing the body with enough calories to allow for tissue healing.
- Target muscle function:
Muscle size and strength seems to be protective of BSIs.
Training for increased strength is indicated, but not at the sake of symptom provocation. Always stay in the pain free zone. Let the pain be your guide.
Target muscles locally (at the site of BSI) and globally (for whole body strength). It will depend upon which type of BSI a patient presents with, that allows for certain exercises, while ruling out others. Usually, exercises that bend the bone in a way that compressed the injured site are more tolerable and those that lead to tensile strain.
For the metatarsals, it is recommended to start with calf raises only after bone tenderness has completely resolved. While other exercises can be started way sooner.
Usually, when you can walk-pain free, you should be able to do a single leg calf raise (cause that's what happens when walking), then once you can do multiple single-leg calf raises, you can add some weight and reduce repetitions. Then advance that into plyometric exercises (start bilaterally, e.g. CMJs with soft landings and then progress towards single leg pogo-hops as the goal exercise).
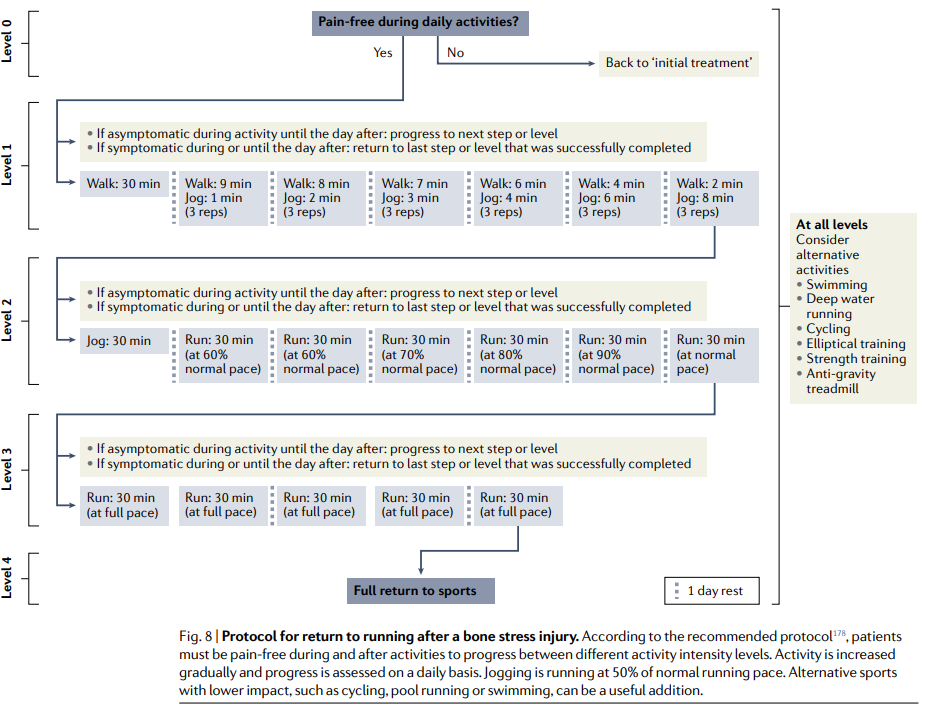
- Return to running:
After leaving the crutches or boot by the side and pain-free walking without external support is possible and ADLs are pain-free for 5 consecutive days, a gradual return to running protocol can be initiated. A walking-running routine will start at around 50% of the runners usual pace, to keep intensity low.
As running intensity strongly determines forces received at the bone, start by first progressing running volume and later running intensity. When increasing intensity, make sure to reduce overall volume in the beginning. In the early stages, running is seen as a modality to load the bones, therefore aerobic capacity should still be maintained via cross training. Progress running time 5-10% each week while monitoring for symptoms.
For more precise return to running criteria and progressions look below.
- Reduce re-injury risk:
Risk factors, such as menstrual dysfunctions in women, decreased BMI (<19) and RED-s should be screened for and addressed, while aiming to optimise running workload. Keep in mind to check for recent changes in running load or running surfaces (e.g. from outdoors to the treadmill).
When it concerns bones, keep in mind to check (or educate) for Vitamin D and Calcium intake and in runners additionally for energy deficiencies.
It is recommended to increase bone strength by adding plyometric / jumping exercises to the program. As these exercises are highly osteogenic (loads can be easily progressed and can be done as an extra session, multiple times a week). Combining plyometrics with resistance training, while increasing running cadence is the standard recommendation for BSI reinjury risk reduction. With cadence being more important on tibial BSIs, while it does not seem to matter for metatarsal ones.
Whats the rationale for increasing bone strength in this population?
When adding resistance training and impact exercise, we aim at increasing bone density. By doing that, bones will strain less from the same external loads and therefore lead to reduced microdamage.
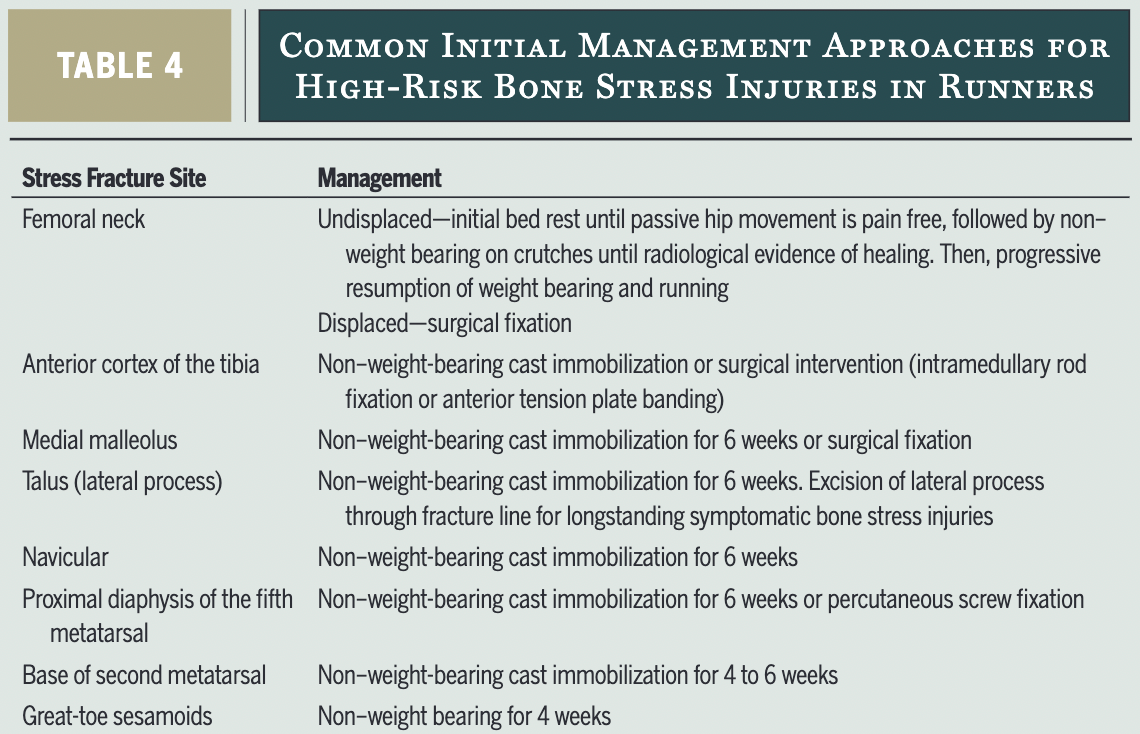
Management of high-risk BSI:
High-risk BSIs are prone to non-union or progression towards complete fracture, if not treated adequately. Return to activity is done with signs of cortical bridging on imaging with pain free palpation (if palpation is possible). Getting an imaging confirmation of healing is an important management difference from low-risk BSIs as well as an initial period of non-weight-bearing (anywhere from 4 to 6 weeks). With a longer healing duration.
Regaining overall conditioning via cross training is crucial in these people. While trying to reduce risk factors associated with BSI development.
The general interventions, such as cueing for "softer landings", increasing stride rate and increasing muscular strength are important once loading is allowed.
MRI findings of stress fractures do not always correlate with symptoms. So it it important to have the clinical diagnosis match with the imaging results to be more certain about the diagnosis.
Bone stress injuries of the lumbar spine are common in cricket fast bowlers. In this population, early MRI is indicated and activity modification / unloading until structural healing (around 4-6 months) is seen on the scan. This approach is recommended for high-level athletes in order to reduce risks of further complications (e.g. spondylolisthesis) (Orchard et al., 2023).
BSI recovery principles:
BSIs are most often experienced by athletes (especially long distance runners). In order to treat them two things are crucial:
#1 load management
#2 increasing bone loading capacity.
As it seems, loading is the cause of injury as well as the groundwork to protect from injury. Optimal bone workload has been defined as "the interaction between the number and magnitude of bone loading cycles that induces adaptation to best enhance function and reduce the risk of re/injury" (Warden et al., 2021).
Without changes in other risk factors, Warden and colleagues state that "there is a linear one-to-one increase in BSI risk for an increase in running volume (i.e., number of loading cycles)" (Warden et al., 2021).
In general, bone stress injuries do not just happen to anyone. They are earned. Through lots of training, beyond ones current capacity.
In the podcast below, researcher Rick Willy, recommends as a rule of thumb, to discern MTSS (medial tibial stress syndrome) from a medial tibial BSI, if pain is spread out over a 10cm area. If its > 10cm, it is 100% MTSS and not a BSI, less than 10 cm you should get an MRI and suspect a BSI.
Another gem was his explanation about the effects of resistance training on bone vs tendons. Usually heavy slow resistance training is used for tendinopathies, to build tendon stiffness, while plyometrics are used to keep athletes jumping, but they don't help increase stiffness. While in bones it's the other way around, where plyometrics actually are great for building bone strength and resistance exercise assists that and helps build muscle to spread the forces. Bone responds best to heavy and fast loading.
Recommended Podcast on all things BSI
What about gait retraining?
That is normally recommended only for people suffering from recurring BSIs, by increasing cadence (strike rate; as this leads to reduced step length which leads to reduced ground reaction forces), cueing softer landings (land like a feather) and potentially transitioning to a fore-foot strike pattern (although the fore-foot pattern does increase stress at the metatarsals and has contradicting findings for tibial loading). Increases in cadence of 5-10% (keeping the same pace, but increasing step-count) should be aimed for.
Can BSIs be prevented? via footwear, foot orthosis (FO) or training related strategies? A 2023 systematic-review and meta-analysis looked at that exact question. They found that "to this day, there is still a lack of evidence regarding BSI prevention with footwear, FOs and training-related strategies." Much more research is needed to find a precise answer to this question, so up until now, investing in expensive footwear or foot orthosis is likely not worth your money.
Getting in more bone work
As seen in the graphic below (in yellow), repetitive bone loading cycles (such as running) only need around 4-8h of recovery until the bone cells can take in more stimuli. This means that in those with low BMD, where we want to increase BMD quickly, another session in the evening of plyometric work might be a good tactic. But as plyometric work needs a recovery time of around 48h, these extra sessions should not be performed daily.

But do not sacrifice rest periods. They are important even for high level athletes (or especially for them). Warden points out that "at least 1 day per week and 1 week every 3 months" of rest should be taken in distance runners at risk of BSI (Warden et al., 2021).
Bone stress reactions (BSR)
A BSR is the precursor of a BSI and is "characterized by increased bone turnover associated with periosteal and/or marrow edema" (Warden et al., 2014).
It is not detectable on MRI or x-ray and a patient experiences symptoms of lower degrees than from an actual BSI. When a BSR can be detected early, then rehab can be abbreviated, while with a late-stage BSR, the rehab will look as with a BSI.
At first it's a stress reaction, but if the demands on the bone continue to exceed its capacity without allowing for recovery, it may result in a stress fracture.A bone stress fracture is established after it is visible radiologically.
Return to running
Return-to-run criteria after tibial BSI: (George et al., 2024)
- Tibial tenderness should be assessed and monitored. Tenderness is allowed in low-risk tibial BSIs (simply monitor for increases in symptoms) but not in high-risk BSIs prior to return to running.
- Pain free walking and ADLs. Walking recommendations wary from 1 mile to 45 min of walking pain free to be allowed to return to running.
- Imaging is needed for high-risk BSIs to confirm healing, but not so in low-risk BSIs, as "radiographs are limited by low sensitivity, particularly in the early stages of stress fracture, and in some cases may not reveal an existing stress fracture at any time".
- Lower extremity strength training should be performed and assessed prior to return to running. For tibial BSIs, perform calf raises. Functional tests, such as the single leg hop can be used to predict the return to pain-free running.
- Address risk factors (nutrition, menstrual health, psychology, training load, energy deficiency, REDs) that led to the BSI in the first place, to reduce likelihood of recurrence. With training load and REDs being of special importance. Screen for REDs using the Low Energy Availability in Females Questionnaire (LEAF-Q), the IOC REDs clinical assessment tool or the Female Athlete Triad Coalition cumulative risk assessment tool. In the case of high risk findings, referral to a specialist is indicated (dietitian, sports medical doctor).
Return-to-run progressions: (George et al., 2024)
- Progress with a walk-run protocol, starting on alternate days. Where walking is gradually substituted with running (see table above for a detailed example). Initially start with 30-60 seconds of running, with adequate recovery, as tibial stress significantly increases when switching from walking to running. Progressions need to be monitored for the presence of pain.
- Progress distance prior to speed. A running distance of 50% of the pre-injury level should be acquired before progressing speed. The authors suggest that "the rate of progression should be individualised and should take into account the pre-injury training status and the severity of the injury" instead of rigidly sticking to the 5-10% rule. Even if thats probably a safe bet. Sometimes it needs to be less and sometimes it might be more. In females, progressions need to be slower than with males.
- Running surfaces and their relevance to reinjury prevention or return to sport significance remains unclear, with conflicting results in the literature.
- In case of recurrent BSIs, address lower limb biomechanics/running technique (such as reduced stride length, increased cadence ...).
- Add strength training to increases muscular strength (as muscles help with shock absorption, reducing forces on the bone). In the later stages, add plyometric exercises to further increase lower limb bone mass, with jumps focusing on accelerated take-off instead of hard landings.
Short note #1: The female athlete triad
The female athlete triad consists of at least one of the following components (De Souza et al., 2014):
- Low energy availability (with or without eating disorders)
- Low bone mineral density (BMD)
- Menstrual dysfunction
The above components are all connected. As energy deficiencies play a role in menstrual dysfunction, and both of them can to reduced BMD. And it seems that all factors alone pose a risk for the development of BSIs.
In general, the triad can be seen as a continuum. Where on one end there is a healthy athlete with optimal energy availability, regular menses and normal BMD, while on the other end, the athlete has amenorrhoea, low energy availability and osteoporosis.
It is important to screen for this condition early on and to intervene, in order to keep it from progressing into long term damages. Referrals to a sports dietician, physician or mental health professional is advised (for those with eating disorders). Most often females participating in sports that are weight sensitive are affected by the condition (where leanness is important).
These athletes often present with a stable body weight, because other physiological components are taking the hit from the low energy availability. So do not get confused about that.
Screening questions for the female athlete triad:
▸ Have you ever had a menstrual period?
▸ How old were you when you had your first menstrual period?
▸ When was your most recent menstrual period?
▸ How many periods have you had in the past 12 months?
▸ Are you presently taking any female hormones (oestrogen, progesterone, birth control pills)?
▸ Do you worry about your weight?
▸ Are you trying to or has anyone recommended that you gain or lose weight?
▸ Are you on a special diet or do you avoid certain types of foods or food groups?
▸ Have you ever had an eating disorder?
▸ Have you ever had a stress fracture?
▸ Have you ever been told you have low bone density (osteopenia or osteoporosis)?
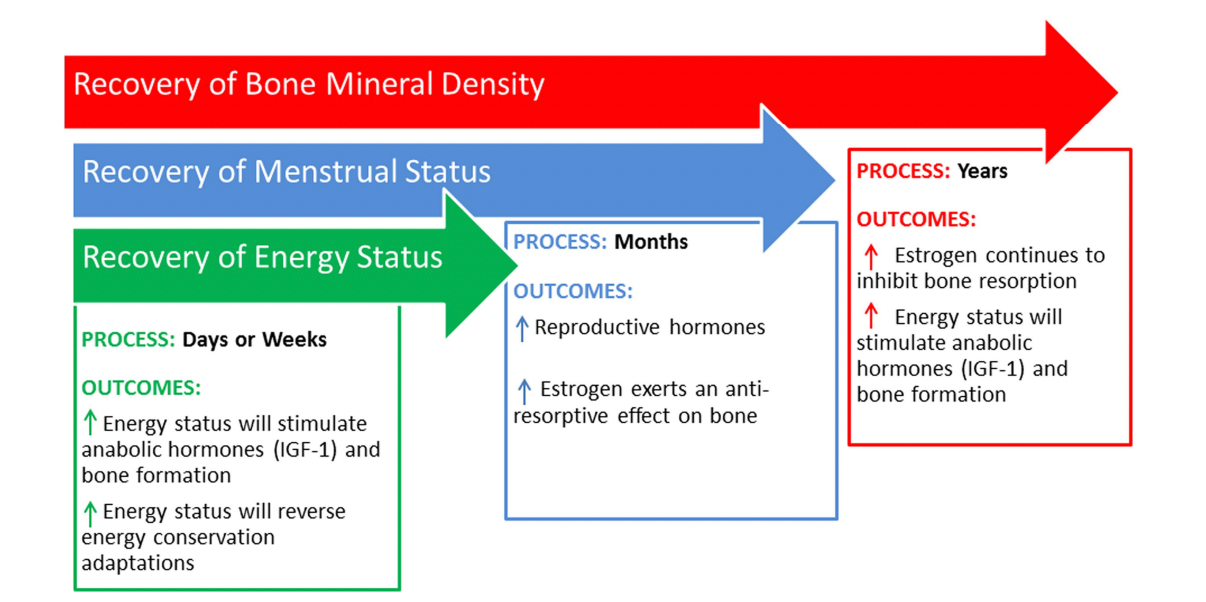
The treatment is going to be multifactorial, with different disciplines working together and a strong focus on increasing energy availability and treating eating disorders, if present. For any significant decreases in BMD that might be present, it is going to take a long time to recover. See image below.
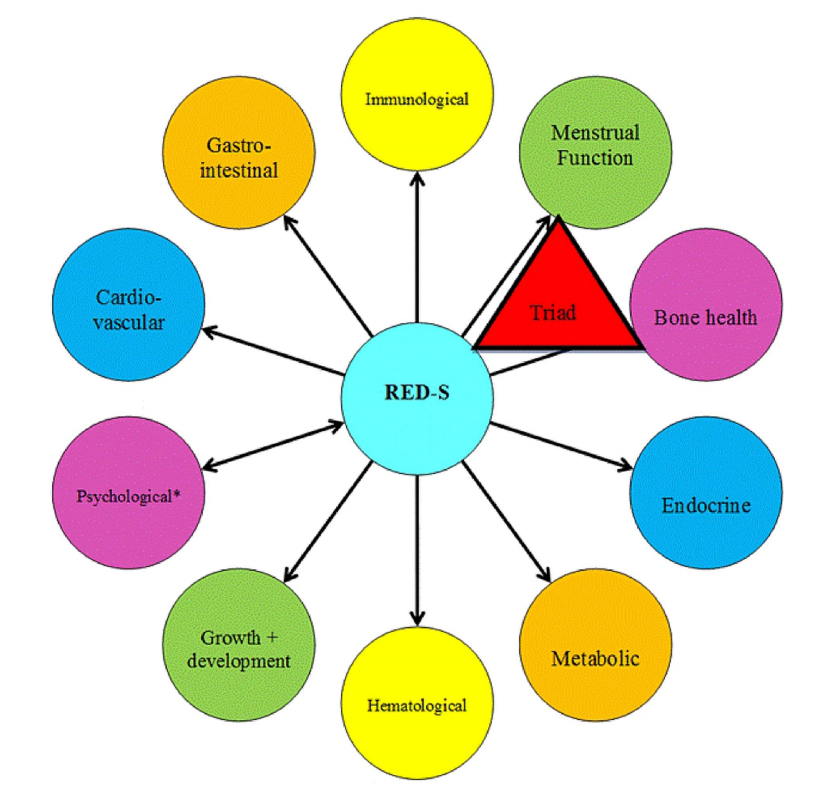
Short note #2: Relative Energy Deficiency in Sport (RED-S)
REDs can be seen as a syndrome that includes the female athlete triad, but is used as a broader term to describe "impaired physiological function including, but not limited to, metabolic rate, menstrual function, bone health, immunity, protein synthesis, cardiovascular health caused by relative energy deficiency" (Mountjoy et al., 2014). Here, men are also included.
So the underlying problem is low energy availability, due to an inadequate intake of energy (calories) or high levels of activity. The body adjusts to the reduced possibility to fuel its systems and this leads to disruptions of various functions. As it takes off from the female athlete triad, REDs includes the triad, but is not limited to it. As other effects such as: Depression, Irritability, Increased injury risk, Decreased muscle strength and coordination, Decreased concentration and more can be affected or caused by REDs. With REDs affecting the following factors:
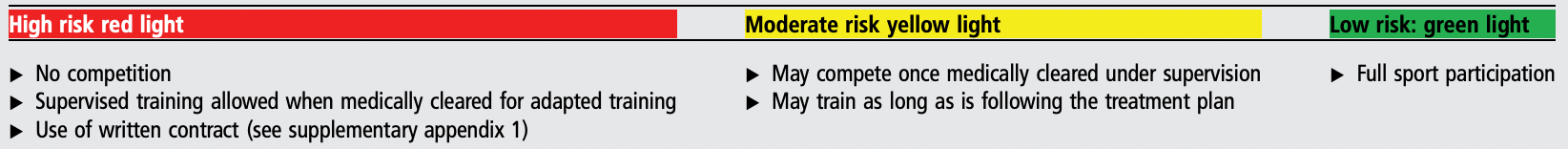
Screening for REDs can be tricky and needs to be done by looking at a variety of factors. Regarding sports participation, exemplary variables are seen below:
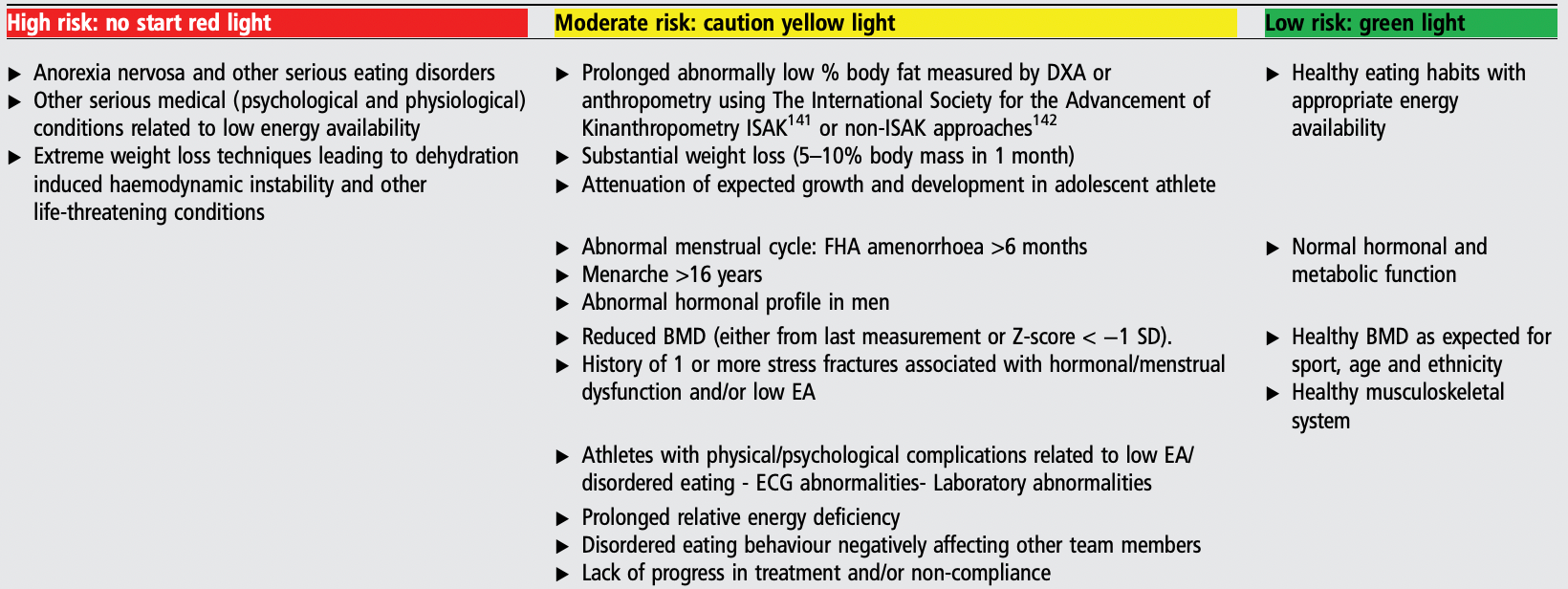
Treating REDs is going to be multifactorial, with a special focus (as in the female athlete triad, on increasing energy availability and target any underlying eating disorders. While trying to increase BMD and making sure the athlete is psychologically in an adequate state.
What about surgery?
In some cases, especially in athletes, surgery might aid with achieving earlier RTS. And may be required for safety reasons in cases like advanced femoral neck BSIs (even if RTS rates are very low afterwards). But, this needs to be a case-by-case decision making process.
References:
De Souza, M. J., Nattiv, A., Joy, E., Misra, M., Williams, N. I., Mallinson, R. J., Gibbs, J. C., Olmsted, M., Goolsby, M., Matheson, G., & Expert Panel. (2014). 2014 Female Athlete Triad Coalition Consensus Statement on Treatment and Return to Play of the Female Athlete Triad: 1st International Conference held in San Francisco, California, May 2012 and 2nd International Conference held in Indianapolis, Indiana, May 2013. British Journal of Sports Medicine, 48(4), 289–289. https://doi.org/10.1136/bjsports-2013-093218
Fredericson, M., Bergman, A. G., Hoffman, K. L. & Dillingham, M. S. (1995). Tibial stress reaction in runners. The American Journal Of Sports Medicine, 23(4), 472–481. https://doi.org/10.1177/036354659502300418
Gabbett, T. J., & Oetter, E. (2024). From Tissue to System: What Constitutes an Appropriate Response to Loading? Sports Medicine (Auckland, N.Z.). https://doi.org/10.1007/s40279-024-02126-w
George, E. R. M., Sheerin, K. R., & Reid, D. (2024). Criteria and Guidelines for Returning to Running Following a Tibial Bone Stress Injury: A Scoping Review. Sports Medicine (Auckland, N.z.), 54(9), 2247–2265. https://doi.org/10.1007/s40279-024-02051-y
Hoenig, T., Ackerman, K. E., Beck, B. R., Bouxsein, M. L., Burr, D. B., Hollander, K., Popp, K. L., Rolvien, T., Tenforde, A. S. & Warden, S. J. (2022). Bone stress injuries. Nature Reviews Disease Primers, 8(1). https://doi.org/10.1038/s41572-022-00352-y
Hoenig, T., Hollander, K., Popp, K. L., Fredericson, M., Kraus, E. A., Warden, S. J. & Tenforde, A. S. (2024). International Delphi consensus on bone stress injuries in athletes. British Journal Of Sports Medicine, bjsports-108616. https://doi.org/10.1136/bjsports-2024-108616
Mountjoy, M., Sundgot-Borgen, J., Burke, L., Carter, S., Constantini, N., Lebrun, C., Meyer, N., Sherman, R., Steffen, K., Budgett, R., & Ljungqvist, A. (2014). The IOC consensus statement: Beyond the Female Athlete Triad—Relative Energy Deficiency in Sport (RED-S). British Journal of Sports Medicine, 48(7), 491–497. https://doi.org/10.1136/bjsports-2014-093502
Orchard, J. W., Saw, R., Kountouris, A., Redrup, D., Farhart, P., & Sims, K. (2023). Management of lumbar bone stress injury in cricket fast bowlers and other athletes. South African Journal of Sports Medicine, 35(1), v35i1a15172. https://doi.org/10.17159/2078-516X/2023/v35i1a15172
Warden, S. J., Davis, I. S., & Fredericson, M. (2014). Management and prevention of bone stress injuries in long-distance runners. The Journal of Orthopaedic and Sports Physical Therapy, 44(10), 749–765. https://doi.org/10.2519/jospt.2014.5334
Warden, S. J., Edwards, W. B., & Willy, R. W. (2021a). Optimal Load for Managing Low-Risk Tibial and Metatarsal Bone Stress Injuries in Runners: The Science Behind the Clinical Reasoning. The Journal of Orthopaedic and Sports Physical Therapy, 51(7), 322–330. https://doi.org/10.2519/jospt.2021.9982
Warden, S. J., Edwards, W. B., & Willy, R. W. (2021b). Preventing Bone Stress Injuries in Runners with Optimal Workload. Current Osteoporosis Reports, 19(3), 298–307. https://doi.org/10.1007/s11914-021-00666-y
Wright, A. A., Hegedus, E. J., Lenchik, L., Kuhn, K. J., Santiago, L. & Smoliga, J. M. (2015). Diagnostic Accuracy of Various Imaging Modalities for Suspected Lower Extremity Stress Fractures. The American Journal Of Sports Medicine, 44(1), 255–263. https://doi.org/10.1177/0363546515574066